
Schizophrenia: beyond clinical remission. Therapeutic challenges to achieving quality of life for each patient
Effective schizophrenia treatment must go beyond clinical remission. It is critical to attain a good quality of life for people with schizophrenia through recovery and preventing relapse.1,2 Recovery should aim to both reduce symptomatic burden and improve social functioning.3 In addition, treatment should be implemented early and persistently,4–7 with effective monitoring to optimize adherence.8 It is also key to individualize treatment by employing patient-focused, multidisciplinary strategies.1,2,9
Recovery of people with schizophrenia should consider clinical remission and broader social functioning3
People with schizophrenia have a high disease burden, involving disability due to symptoms and cognitive impairment, as well as social impairment.5 Clinical remission is defined as a rating of 'mild' or less on key positive and negative symptoms for over 6 months;10 however, comprehensive clinical improvement should include social and functional criteria, such as successful relationships, ability to work, and independent living.11 No generally accepted definition of recovery in schizophrenia has yet been defined, but the following definition has been proposed: Both clinical and social improvements, with at least one of these outcomes lasting 2 years or more.3
Early and uninterrupted treatment of schizophrenia is critical to slow disease progression4–6
Prior to recognition and initiation of treatment, the mean duration of untreated psychosis (DUP) is approximately 15 months.6 Longer DUP is associated with poorer long-term outcomes, in terms of poor general symptomatic outcome, more severe positive and negative symptoms, failure to achieve remission, and decreased social functioning and global outcome.6 This highlights the importance of early diagnosis and treatment of schizophrenia.
Moreover, relapse rates are high among individuals who discontinue antipsychotic medication.7 While many individuals with a first episode of psychosis experience remission within a year of treatment, 77% of those who discontinue antipsychotic medication afterwards relapse within 1 year and 90% relapse within 2 years, compared with just 3% of those who maintain antipsychotic therapy.7 This highlights the importance of persistent treatment to improve long-term outcomes for people with schizophrenia.

Early intervention has established short-term benefits for people with schizophrenia12
Early intervention for schizophrenia involves identification of patients who are already in the prodromal phase or during early psychosis13 and initiation of early, phase-specific treatments, such as cognitive behavioral therapy, antipsychotic medication, and psychological support of family and caregivers.9 The goal is to prevent progression to psychosis in the prodromal phase or promote recovery from a first episode of psychosis.13 Short-term benefits include less severe symptoms, less treatment discontinuation and fewer psychiatric hospitalizations.12 Early intervention is already established in America, Europe, and Australasia.13
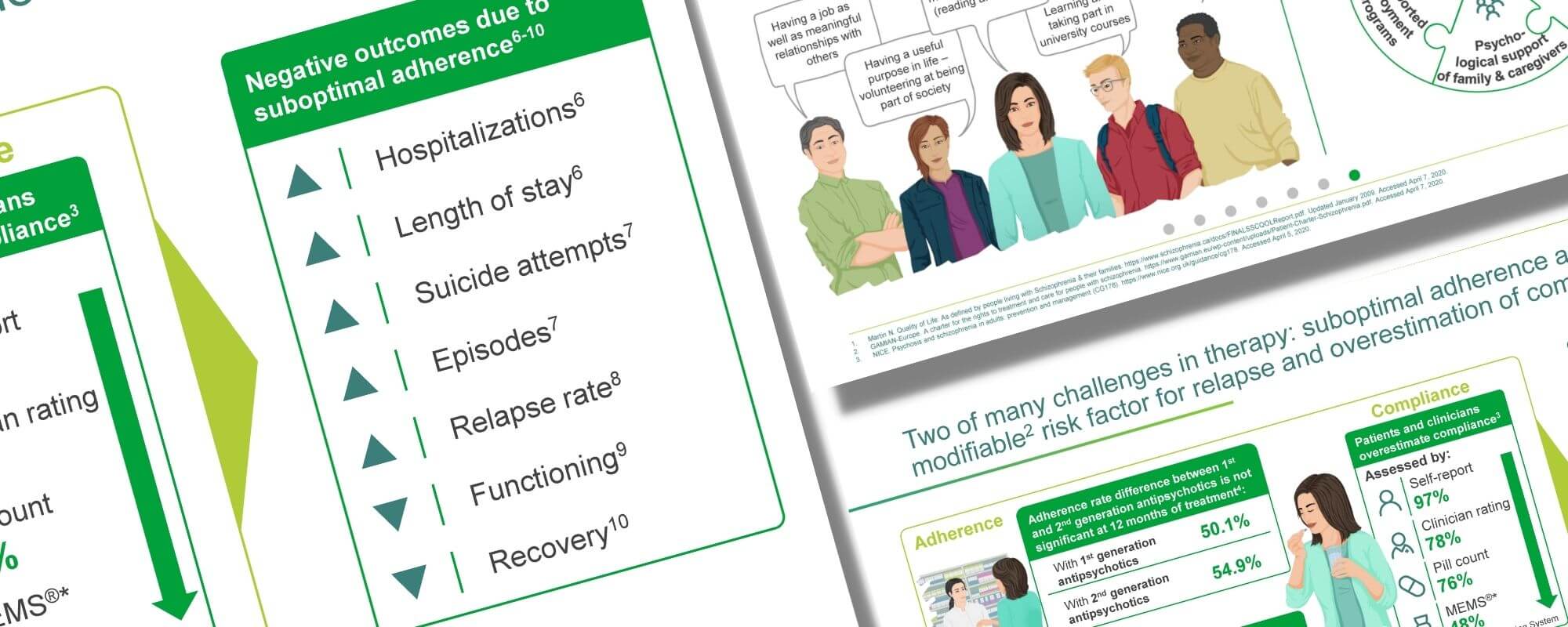
Suboptimal adherence and overestimation of compliance are just two key challenges of schizophrenia treatment14,15
Almost three-quarters of individuals with chronic schizophrenia discontinue their medication within 18 months due to inefficacy, side effects, or other reasons.14 Moreover, both patients and clinicians overestimate compliance.15 As suboptimal adherence negatively impacts patient outcomes,16–20 experts recommend the optimal approach is uninterrupted treatment where compliance is verifiable by a clinician.8
Management of schizophrenia should aim for good quality of life1,2
The goals of schizophrenia management go beyond clinical remission. It is critical to attain a good quality of life through recovery1 and to prevent relapse.2 Therefore, establishing an alliance with the individual is important so that multidisciplinary interventions can be tailored towards their personal concept of a good quality of life.1,2
Martin N. Quality of Life: As defined by people living with Schizophrenia & their families. https://www.schizophrenia.ca/docs/FINALSSCQOLReport.pdf. Updated January 2009. Accessed October 1, 2021.
GAMIAN-Europe. A charter for the rights to treatment and care for people with schizophrenia. https://www.gamian.eu/wp-content/uploads/Patient-Charter-Schizophrenia.pdf. Accessed October 1, 2021.
Jääskeläinen E, Juola P, Hirvonen N, et al. A systematic review and meta-analysis of recovery in schizophrenia. Schizophr Bull 2013;39:1296–1306.
Millan MJ, Andrieux A, Bartzokis G, et al. Altering the course of schizophrenia: progress and perspectives. Nat Rev Drug Discov 2016;15:485–515.
Fleischhacker WW, Arango C, Arteel P, et al. Schizophrenia—time to commit to policy change. Schizophr Bull 2014;40 Suppl 3:S165–S194.
Penttilä M, Jääskeläinen E, Hirvonen N, et al. Duration of untreated psychosis as predictor of long-term outcome in schizophrenia: systematic review and meta-analysis. Br J Psychiatry 2014;205:88–94.
Zipursky RB, Meneze NM, Streiner DL, et al. Risk of symptom recurrence with medication discontinuation in first-episode psychosis: a systematic review. Schizophr Res 2014;152:408–414.
Shirley M, Perry CM. Aripiprazole (ABILIFY MAINTENA®): a review of its use as maintenance treatment for adult patients with schizophrenia. Drugs 2014;74:1097–1010.
NICE. Psychosis and schizophrenia in adults: prevention and management (CG178). https://www.nice.org.uk/guidance/cg178. October 1, 2021.
Andreasen NC, Carpenter WT, Kane JM, et al. Remission in schizophrenia: proposed criteria and rationale for consensus. Am J Psychiatry 2005;162:441–449.
Jääskeläinen E, Juola P, Hirvonen N, et al. A systematic review and meta-analysis of recovery in schizophrenia. Schizophr Bull 2013;39:1296–1306. Supplementary data. Available at: https://academic.oup.com/schizophreniabulletin/article/39/6/1296/1884290#supplementary-data. Accessed October 1, 2021.
Correll CU, Galling B, Pawar A, et al. Comparison of early intervention services vs treatment as usual for early-phase psychosis: a systematic review,meta-analysis, and meta-regression. JAMA Psychiatry 2018;75:555–565.
Marshall M, Rathbone J. Early intervention for psychosis (Review). Cochrane Database Syst Rev 2011;6:CD004718.
Lieberman JA, Stroup TS, McEvoy JP, et al. Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. N Engl J Med 2005;353:1209–1223.
Remington G, Kwon J, Collins A, et al. The use of electronic monitoring (MEMS®) to evaluate antipsychotic compliance in outpatients with schizophrenia. Schizophr Res 2007;90:229–237.
Ascher-Svanum H, Zhu B, Faries DE, et al. Medication adherence levels and differential use of mental-health services in the treatment of schizophrenia. BMC Res Notes 2009;2:6.
Ahn J, McCombs JS, Jung C, et al. Classifying patients by antipsychotic adherence patterns using latent class analysis: characteristics of nonadherent groups in the California Medicaid (Medi-Cal) Program. Value Health 2008;11:48–56.
Morken G, Widen JH, Grawe RW. Non-adherence to antipsychotic medication, relapse and rehospitalisation in recent-onset schizophrenia. BMC Psychiatry 2008;8:32.
Dassa D, Boyer L, Benoit M, et al. Factors associated with medication non-adherence in patients suffering from schizophrenia: a cross-sectional study in a universal coverage health-care system. Aust N Z J Psychiatry 2010;44:921–928.
Novick D, Haro JM, Suarez D, et al. Recovery in the outpatient setting: 36-month results from the Schizophrenia Outpatients Health Outcomes (SOHO) study. Schizophr Res 2009;108:223–230.