
Modern understanding of the pathophysiology of migraine
Migraine is a specific type of headache that involves multiple regions of the brain,1 and is normally associated with other symptoms such as nausea, vomiting, photophobia, phonophobia, and cutaneous allodynia.2 A migraine attack can be typically divided into four phases: the premonitory phase (preceding the headache); the aura phase (immediately preceding or accompanying the headache); the headache phase; and the postdrome phase (after the headache is resolved).3,4 These phases can overlap, and some migraine symptoms could be experienced during all four phases.
The field of research in migraine pathophysiology has historically been dominated by two main theories—the vascular theory and the neuronal theory. The former considered abnormal vasodilation in the brain as the main cause of migraine.5 However, advances during the past few decades have shown that vascular changes are neither necessary nor sufficient to explain the pain associated with migraine.4,6,7 In this timeframe, the neuronal theory has progressively gained credibility, and the focus of migraine research has shifted to specific brain structures thought to be at the basis of the migraine headache.
Our understanding of the pathophysiology and anatomy relevant to migraine has evolved along with progress in the fields of migraine genetics and advanced imaging. It is now widely accepted that there is no unique “migraine generator” involved in the pathophysiology of migraine.1,8 Rather, the variety and overlap of the different phases and different symptoms and signs of migraine should be viewed in light of a complex multifactorial brain network disorder, involving multiple cortical, subcortical, and brainstem regions of the brain.1,8
The anatomy of the migraine brain
The key to understanding migraine pathophysiology lies in the way different neural networks interact with each other. The headache phase of migraine correlates with the activity of the trigeminovascular system, which relays nociceptive information from the meninges to the brain.1,7 This system consists of a plexus of peripheral axons that extends from the trigeminal ganglion, and innervate the meninges and their vasculature (Figure 1).7 Centrally, the plexus converges in the trigeminocervical complex (TCC) of the brainstem.1,7 Signals relayed through the TCC are the likely cause of migraine pain and other symptoms such as photophobia and nausea.4 Furthermore, inputs from the ophthalmic division of the trigeminal nerve and the dural vasculature are strongly associated with the perception of pain.4,7,9
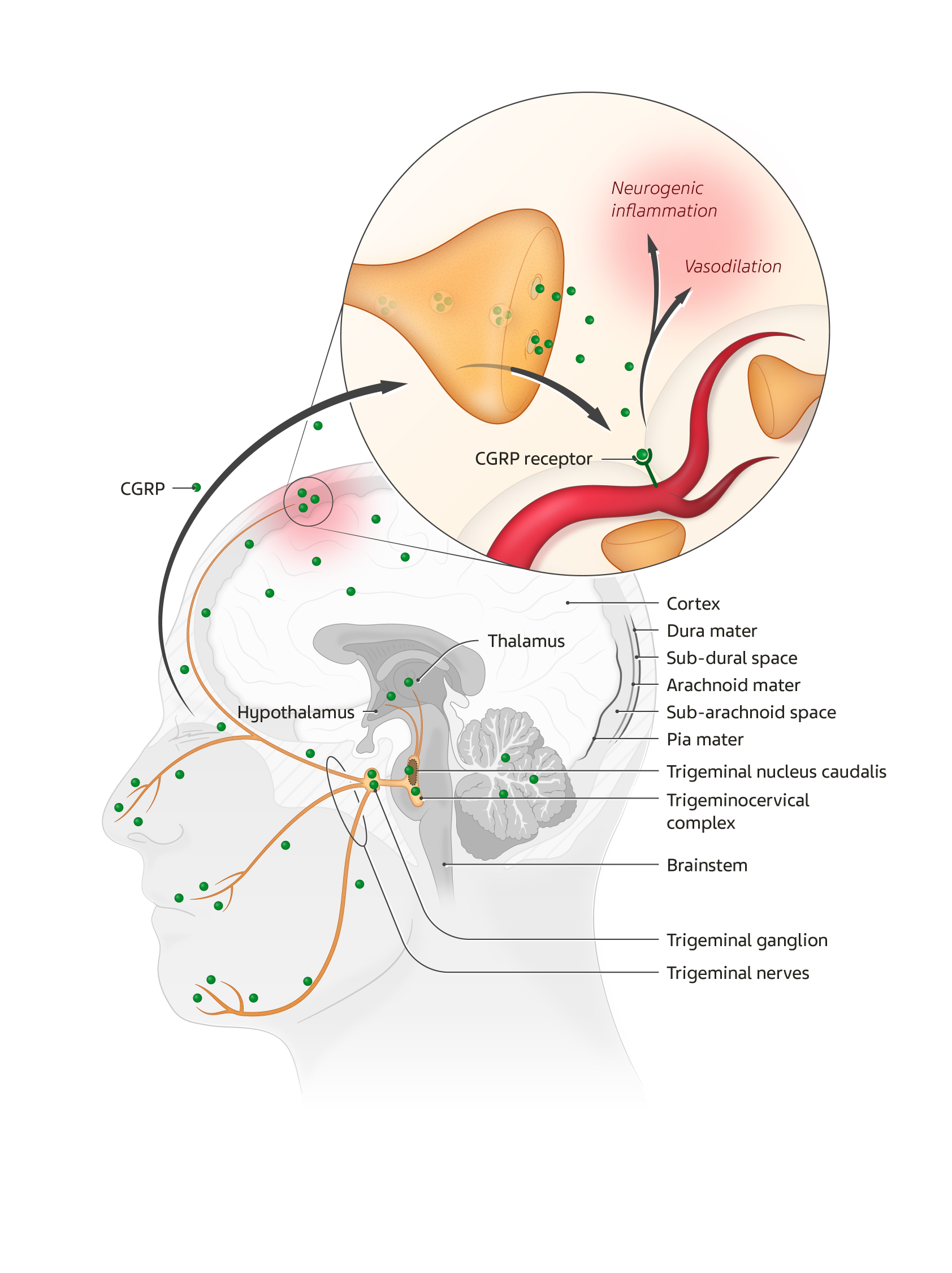
Figure 1. The anatomy of the migraine brain
The TCC consists of the trigeminal nucleus caudalis (TNC) and the dorsal horn of the C1–C2 segments of the spinal cord.1,7 From these, multiple functional connections project to other key areas involved in processing pain, such as the thalamus, hypothalamus, and brainstem nuclei (Figure 1).1,7 Imaging studies have shown that these areas are also activated before and after pain symptoms appear, which suggests that their involvement is not limited to conveying nociceptive signals.7
Trigeminal nerve endings contain vasoactive neuropeptides such as calcitonin gene-related peptide (CGRP), substance P, neurokinin A, and pituitary adenylate-cyclase activating peptide (PACAP).4 Activation of these neurons triggers the release of the neuropeptides, especially CGRP, leading to neurogenic inflammation, and vasodilation of dural and pial vessels (Figure 1). While vasodilation does not directly cause migraine, and neurogenic inflammation is unlikely to be a major migraine trigger, the latter may be involved in the sensitization of peripheral nociceptors.4,10 CGRP is also likely involved in central nociceptive sensitization.4,10 Although the exact mechanism of migraine onset remains to be elucidated, CGRP is clearly involved in modulating nociceptive input to the TCC.1,10,11
CGRP as a mediator of migraine
Several studies in the past two decades have shown that CGRP plays a key role in migraine pathogenesis.10 Clinical evidence supporting this conclusion includes: elevated levels of CGRP in the circulation during migraine attacks; development of migraine-like headaches after experimental injection of CGRP; and effectiveness of selective CGRP receptor antagonists in the treatment of migraine.10,11
In addition to nociceptive modulation and pain perception, CGRP is likely involved in other migraine phases and phenomena, such as photophobia and migraine aura.10 The mechanism through which CGRP causes migraine aura is believed to be related to its critical role in cortical spreading depression (CSD).7,10
There are several potential sites of action of CGRP. This neuropeptide is widely expressed throughout the peripheral and central nervous systems, and is particularly enriched throughout the trigeminovascular system (Figure 1).7 In the periphery, CGRP activates receptors on smooth muscle cells in the dural blood vessel walls. Centrally, it mediates pain transmission via second- and third-order neurons.7 Stimulation of the brainstem activates the trigeminovascular system and causes CGRP to be released peripherally.7
CGRP acts on the canonical CGRP receptor complex, which consists of the calcitonin receptor-like receptor (CLR)—a receptor with seven transmembrane domains—and a single transmembrane protein called receptor activity-modifying protein 1 (RAMP1).4,7 CGRP also activates a second receptor, the amylin receptor (AMY), which combines the calcitonin receptor (CTR) and RAMP1.4,10 However, this noncanonical CGRP receptor likely plays a lesser role in migraine.10
Promising developments in the treatment of migraine
With a better understanding of migraine pathophysiology, the focus of research has shifted to target-based approaches.7 In this context, the CGRP pathway has emerged as one of the primary mediators of migraine.10 In recent years, several monoclonal antibodies targeting the CGRP pathway have been studied and approved in select global regions for preventive treatment of episodic and chronic migraine.7 In light of this, the first oral gepant, or small CGRP receptor antagonist, was recently approved in the US for the acute treatment of migraine attacks.12 The development of new treatments targeting the CGRP pathway represents an exciting progress in the field of migraine prevention.
Puledda F, Messina R & Goadsby PJ. An update on migraine: current understanding and future directions. Journal of Neurology. 2017;264:2031-2039.
Headache Classification Committee of the International Headache Society (IHS). The International Classification of Headache Disorders, 3rd edition. Cephalalgia. 2018;38:1-211.
Charles A. The pathophysiology of migraine: implications for clinical management. The Lancet Neurology. 2018;17:174-182.
Goadsby PJ, Holland PR, Martins-Oliveira M, Hoffmann J, Schankin C & Akerman S. Pathophysiology of Migraine: A Disorder of Sensory Processing. Physiol Rev. 2017;97:553-622.
Ho TW, Edvinsson L & Goadsby PJ. CGRP and its receptors provide new insights into migraine pathophysiology. Nat Rev Neurol. 2010;6:573-582.
Amin FM, Asghar MS, Hougaard A, Hansen AE, Larsen VA, de Koning PJ, Larsson HB, Olesen J & Ashina M. Magnetic resonance angiography of intracranial and extracranial arteries in patients with spontaneous migraine without aura: a cross-sectional study. Lancet Neurol. 2013;12:454-461.
Ong JJY, Wei DY-T & Goadsby PJ. Recent Advances in Pharmacotherapy for Migraine Prevention: From Pathophysiology to New Drugs. Drugs. 2018;78:411-437.
Borsook D & Burstein R. The enigma of the dorsolateral pons as a migraine generator. Cephalalgia. 2012;32:803-812.
Akerman S, Holland PR & Goadsby PJ. Diencephalic and brainstem mechanisms in migraine. Nature Reviews Neuroscience. 2011;12:570-584.
Russo AF. Calcitonin gene-related peptide (CGRP): a new target for migraine. Annu Rev Pharmacol Toxicol. 2015;55:533-552.
Gingell JJ, Hendrikse ER & Hay DL. New Insights into the Regulation of CGRP-Family Receptors. Trends Pharmacol Sci. 2019;40:71-83.
Dubowchik GM, Conway CM, & Xin AW. Blocking the CGRP Pathway for Acute and Preventive Treatment of Migraine: The Evolution of Success. J Med Chem 2020;63(13):6600-6623.